SARS cov 2 COVID 19
>COVID19 pneumonia
>Peep Protocol Video
>R/I Ratio Method Video
>Tutorial for Prone Position
>Lung Echography
COVID19 pneumonia
Protocols for Covid 19 infection with severe acute hypoxemia and respiratory distress Syndrome.
First we test a PEEP between 7-10 cmH20, if PF> 200 we stay like this.
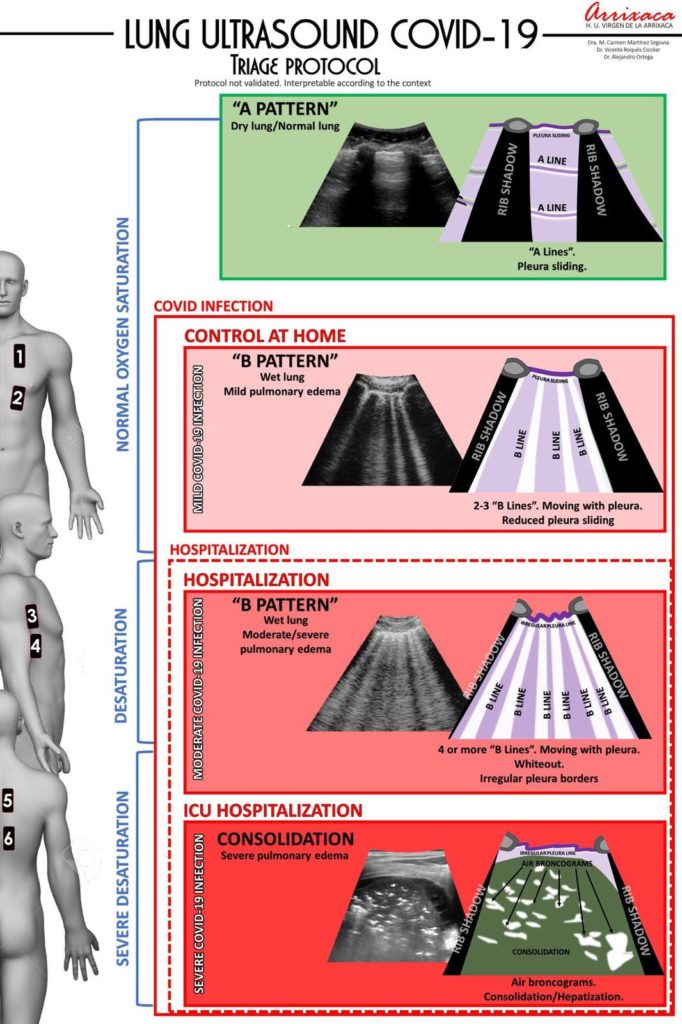
If PF < 150, we see patients with or without consolidations in the dependent lung (Chest CT scan and Pulmonary Echography). This might help to select the protocol (PEEP, Prone, NO, ECMO…).
Patients with lower compliance (consolidations) have higher recrutability assessed by Recrutment/Inflation ratio and response to prone position. Pan et al. AJRCCM 2020
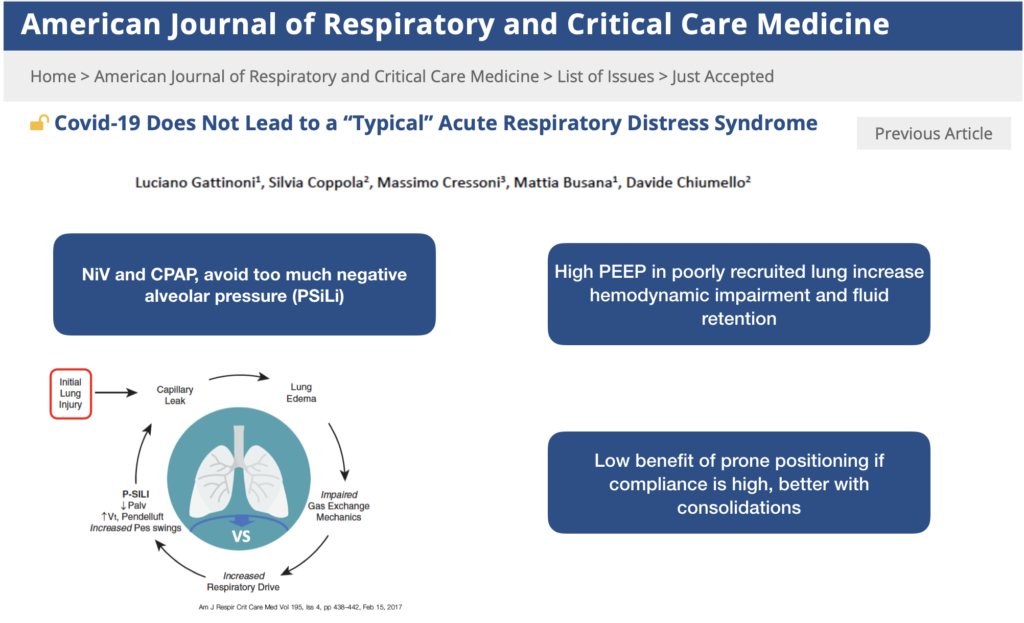
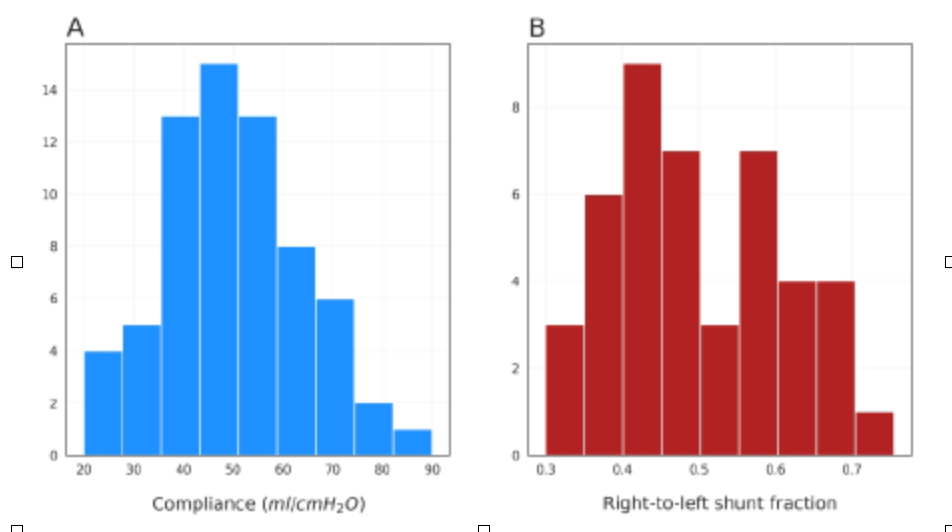
Some patients are very hypoxemic with normal compliance (Echography of the lungs B lines, edema, peripheral ground-glass on CT scan) whereas others have more classical ARDS with consolidations and lower compliance (Echography of the lungs, C Lines, dependent lung) . It is important that patients with high PEEP level (14-20) are responders with higher PaO2/FiO2 +/- alveolar recruitability (R:I ratio >0,5) and without cardiac output impairment and hypotension. If compliance of the respiratory system is >50 ml/cmH2O they probably need less PEEP around 10-13 cmH2O and Pplat of 25 cmH2O (low recrutability (R:I ratio <0,5) , however you can test the effect of PEEP on the intrapulmonary shunt. It can be assessed with the gradient ETCO2/PaCO2.This gradient can be helpful to assess ventilation/perfusion mismatch with intra pulmonary shunt and/or dead space in ARDS. Covid+ patients with significant ground glass on CT scan and high hypoxemia have shunt around 50%. With a shunt > 50% PaO2 will poorly respond to an increase of FiO2.
The further away from 1, the greater the dead space and/or shunt. Avoid high PEEP if there is no physiological effect on shunt or PF ratio, this will avoid fluid retention.
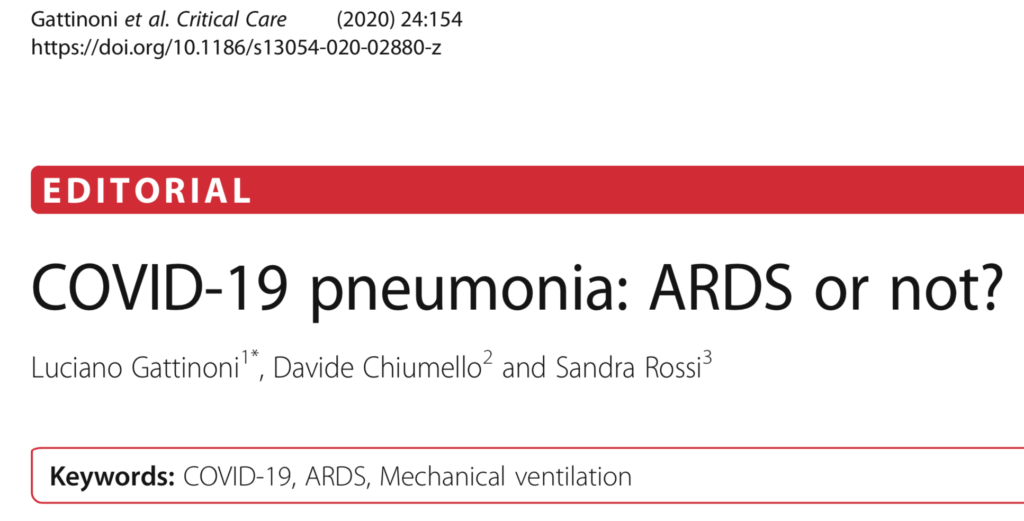
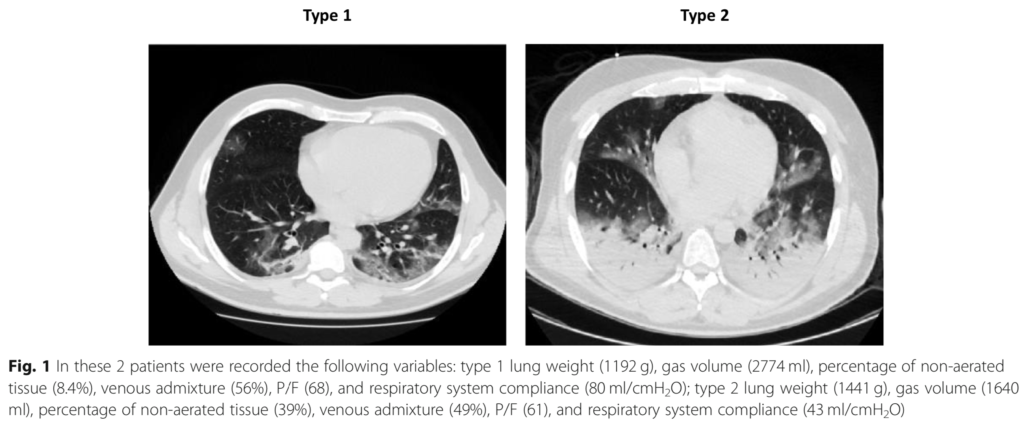
With normal compliance (Type 1 on the CT scan above), Driving Pressure will be low (<10). PEEP/FiO2 tables will propose high level of PEEP. In classical ARDS the level of PEEP in severe patients is often limited by the plateau pressure, because the compliance is lower in these patients (type 2 on the Ct scan above). High PEEP with high compliance (Type 1) can lead to high end expiratory lung volume (EELV) whereas the lungs are already full of gas with normal compliance and low recrutability. The side effect of PEEP if PaO2 does not increase is hyperinflation with hemodynamic impairment (especially in case of hypovolemia, fever, diarrhea ..) and with time high PEEP can lead to fluid retention.
The physiopathology of this shunt in type 1 is not clear but a recent study with autopsy of Covid-19 patients compared to 2009 H1N1 patients is interesting in the NEJM.
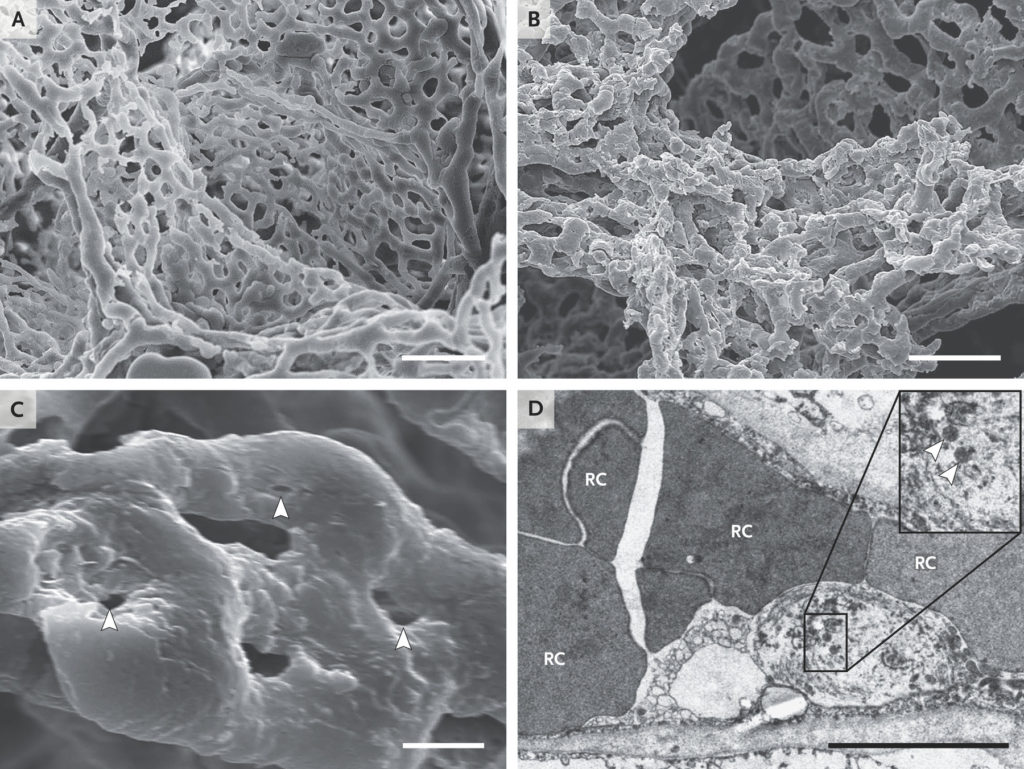
Panels A and B show scanning electron micrographs of microvascular corrosion casts from the thin-walled alveolar plexus of a healthy lung (Panel A) and the substantial architectural distortion seen in lungs injured by Covid-19 (Panel B). The loss of a clearly visible vessel hierarchy in the alveolar plexus is the result of new blood-vessel formation by intussusceptive angiogenesis. Panel C shows the intussusceptive pillar localizations (arrowheads) at higher magnification. Panel D is a transmission electron micrograph showing ultrastructural features of endothelial cell destruction and SARS-CoV-2 visible within the cell membrane (arrowheads) (the scale bar corresponds to 5 μm). RC denotes red cell. From Ackermann et al. NEJM 2020.
Screen simulation PEEP and Type 1
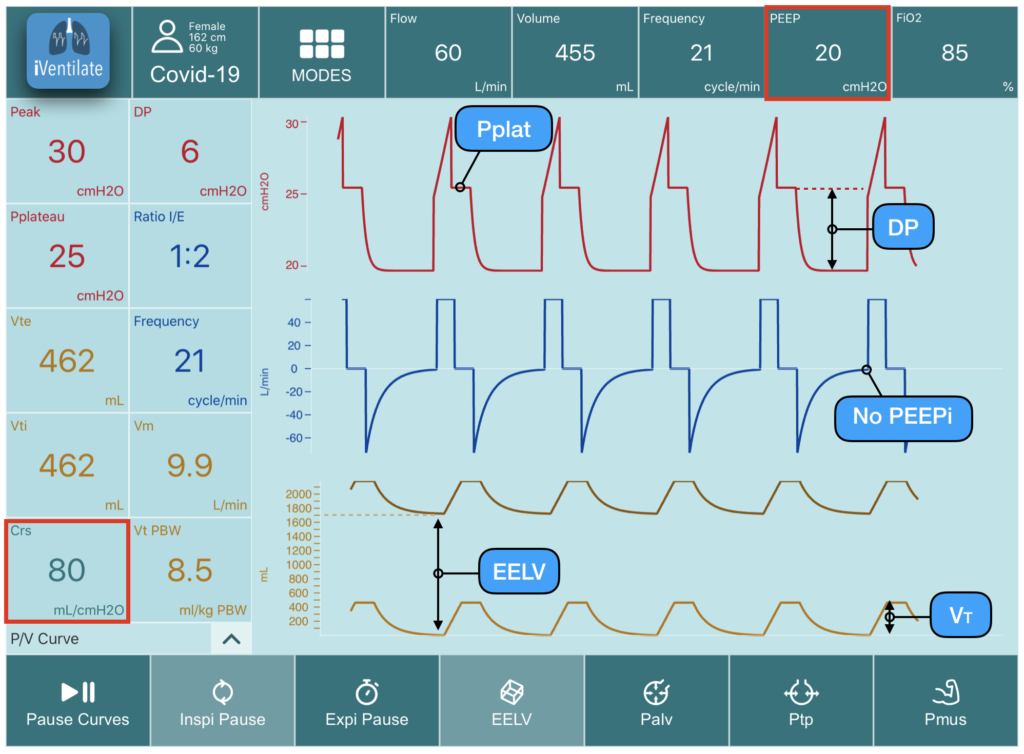
Here the simulated patient has severe hypoxemia (venous admixture) requiring high FiO2 (85%). Compliance of the respiratory system is high at 80 ml/cmH2O. With a PEEP of 20 cmH2O, Pplat is 25 cmH2O and DP is 6 cmH2O. PEEP increases significantly EELV to 1700 ml in a woman of 162 cm (high inflation high EELV in proportion to her functional residual capacity). The effect of such high level of PEEP can impair hemodynamic function. Moreover if RI ratio is below 0,5 it means that the increase of EELV goes essentially in the non dependent lung already aerated.
It is possible to test inhaled NO in patients with severe hypoxemia and high compliance (high shunt) , we challenge in that case the perfusion mismatch of the VA/Q, some will also test almitrine ?).
Because of the shunt you don’t need to let high FiO2, test lower FiO2 for SaO2 around 90-92%. Don’t forget that pulmonary embolism is frequent. If compliance is lower (<40) and PF<150 it might be relevant to titrate more PEEP with a Pplat of 28-30 cmH2O and if PF remains below 150 you can try prone position. Prone seems to work better with consolidations, oxygenation improve, not always, but it can be also beneficial in term of ventilator induce lung injury reduction.
In patient with high shunt, normal compliance and low recrutability (R/I<0,5), PEEP might still be beneficial on oxygenation without cardiac output impairment. This can be explained by perfusion mismatch, the idea is that PEEP will reduce the abnormal high flow of ground glass injury (like a vasoconstriction effect) and then improves oxygenation. It is possible that this persistent high flow (explains the shunt effect) and is the consequence of pulmonary vasoconstriction inhibition by the local viral injury. Studies are required to confirm and explain such pathophysiology ?
Patients with lower compliance (consolidations, type 2) have higher recrutability assessed by R/I with prone position. Pan et al. AJRCCM 2020
Below a video of ventilator setting to illustrate the Express protocol application. This simple protocol* helps to titrate PEEP individually in case of severe ARDS with low compliance, alveolar recrutability (R/I ratio>0,5) and PF<150 (Mercat et al.JAMA 2008) associated with prone position if PF remains <150 with PEEP (Guerin et al. NEJM 2013).
Peep Protocol Video
Patient with severe hypoxemia PF<150 and low compliance < 45, Type 2 or phenotype High, as described by Gattinoni et al.
R/I Ratio Method Video
Below this video below explains a method to measure the recruitment to Inflation ratio proposed by the group of Toronto to assess lung recruitability vs distension at the bedside. For simplicity we test and compare 2 levels of PEEP 5 and 15 cmH2O, then the drop is 10 cmH2O, easier to do the math with this method. This idea is to decide wether high PEEP is necessary in term of alveolar recruitment or not. If you have 16 of PEEP in a severe ARDS with a R/I<0,5 you should try to reduce PEEP to 12 cmH2O and check oxygenation.
This method has been used to assess recrutability in SAR Cov2 associated ARDS by Beloncle et al. and found interesting results. In 25 patients with SARS-Cov-2 associated ARDS, 64% were considered as highly recruitable (RI >0,5) and only 36% as poorly recruitable (RI<0,5) the R/I ratio was performed on the day of intubation. This observation suggests that a systematic R/I ratio assessment may help to guide initial PEEP titration to limit harmful effect of unnecessary high PEEP in the context of Covid-19 crisis.
Tutorial for Prone Position
Find here the Tutorial from Guerin et al. NEJM for prone position
Lung Echography
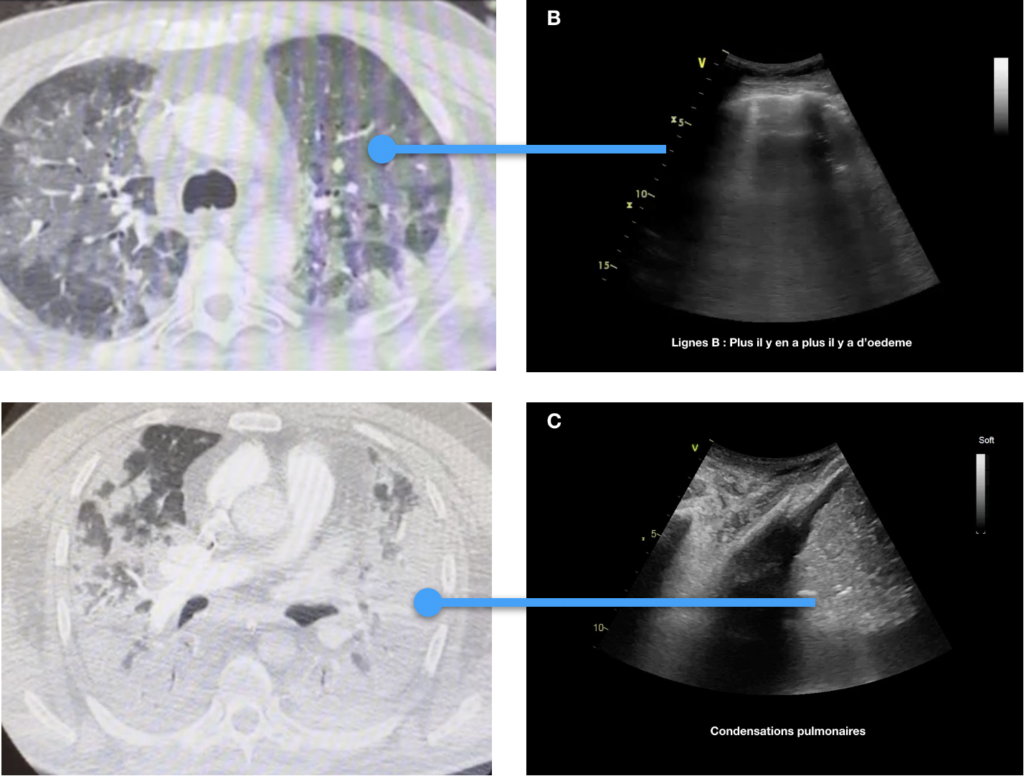
Videos of lung echography with normal A line, pulmonary interstitial lung oedema B line, and consolidations. We check every day the Lungs the Heart and we look for vascular thrombosis.